5.1
Biological Rhythms: The Tides of Experience
Are you an “early bird” or a “night owl”? Do you feel more energized at 5:00 in the morning or at 5:00 at night? Do you have a hard time revving up in the morning or winding down at night? Your answers to these questions may reflect how you respond to the complex interplay of your bodily systems' ups and downs as you progress through the day. In this section, we will take a look at the internal tempos and natural cycles our bodies regularly go through.
Circadian Rhythms
The human body goes through dozens of ups and downs in physiological functioning over the course of a day, a week, and a year, changes that are known as biological rhythms. A biological clock in our brains governs the waxing and waning of hormone levels, urine volume, blood pressure, and even the responsiveness of brain cells to stimulation. Biological rhythms are typically in tune with external time cues, such as changes in clock time, temperature, and daylight, but many rhythms continue to occur even in the absence of such cues; they are endogenous, or generated from within.
Circadian rhythms are biological rhythms that occur approximately every 24 hours. They evolved in plants, animals, insects, and human beings as an adaptation to the many changes associated with the rotation of Earth on its axis, such as changes in light, air pressure, and temperature. The best-known circadian rhythm is the sleep–wake cycle, but hundreds of others affect physiology and performance. Body temperature fluctuates about 1 degree centigrade each day, peaking, on average, in the late afternoon and hitting a low point, or trough, in the wee hours of the morning. Other rhythms occur less frequently than once a day—say, once a month or once a season. In the animal world, seasonal rhythms are common. Birds migrate south in the fall, bears hibernate in the winter, and marine animals become active or inactive, depending on bimonthly changes in the tides. Some seasonal and monthly rhythms also occur in humans. In both men and women, testosterone peaks in the autumn and dips in the spring (Stanton, Mullette-Gillman, & Huettel, 2011), and in women, the menstrual cycle occurs roughly every 28 days. Other rhythms occur more frequently than once a day, many of them on about a 90-minute cycle. In humans, these include physiological changes during sleep, and (unless social customs intervene) stomach contractions, hormone levels, susceptibility to visual illusions, verbal and spatial performance, brain-wave responses during cognitive tasks, and daydreaming (Blumberg, Gall, & Todd, 2014; Escera, Cilveti, & Grau, 1992; Klein & Armitage, 1979; Lavie, 1976).
In most societies, clocks and other external time cues abound, and people's circadian rhythms become tied to them, following a strict 24-hour schedule. Therefore, to identify endogenous rhythms, scientists isolate volunteers from sunlight, clocks, environmental sounds, and all other cues to time. Some hardy souls have spent weeks isolated in underground caves; usually, however, participants live in specially designed rooms equipped with audio systems, comfortable furniture, and temperature controls. Free of the tyranny of a timepiece, a few of these people have lived a “day” that is much shorter or longer than 24 hours. If allowed to take daytime naps, however, most soon settle into a day that averages 5 to 10 minutes longer than 24 hours (Duffy et al., 2011). For many people, alertness, like temperature, peaks in the late afternoon and falls to a low point in the very early morning (Lavie, 2001).
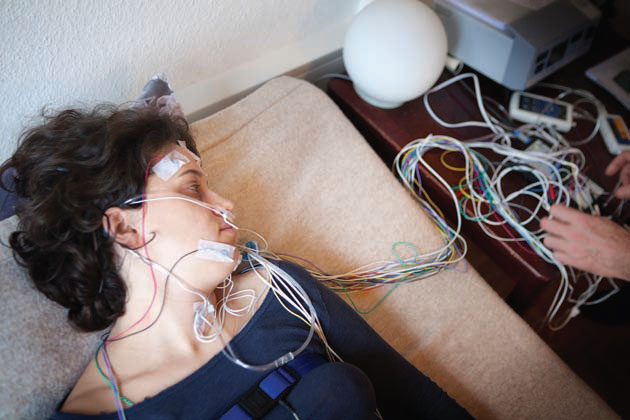
A person participating in a sleep study will be asked to spend a night in a sleep laboratory, often attached to various recording devices that measure physiological and brain activity throughout the night. After a period of adjustment, most people find they can drift off for the night despite these unusual circumstances.
The Body's Clock Circadian rhythms are controlled by a biological clock, or overall coordinator, located in a tiny cluster of cells in the hypothalamus called the suprachiasmatic nucleus (SCN). Neural pathways from special receptors in the back of the eye transmit information to the SCN and allow it to respond to changes in light and dark. The SCN then sends out messages that cause the brain and body to adapt to these changes. Other clocks also exist, scattered around the body, but for most circadian rhythms, the SCN is regarded as the master pacemaker.
The SCN regulates fluctuating levels of hormones and neurotransmitters, and they in turn provide feedback that affects the SCN's functioning. During the dark hours, one hormone regulated by the SCN, melatonin, is secreted by the pineal gland, deep within the brain. Melatonin induces sleep. When you go to bed in a darkened room, your melatonin level rises; when light fills your room in the morning, it falls. Melatonin, in turn, appears to help keep the biological clock in phase with the light–dark cycle (Haimov & Lavie, 1996; Houdek et al., 2015). What's more, melatonin treatments have been used to regulate the disturbed sleep–wake cycles of blind people who lack light perception and whose melatonin production does not cycle normally (Flynn-Evans et al., 2014). The video Rhythms of Consciousness provides more information on how the brain regulates sleep-wake cycles.
Watch
Rhythms of Consciousness
When the Clock Is Out of Sync Under normal conditions, the rhythms governed by the SCN are in phase with one another. Their peaks may occur at different times, but if you know when one rhythm peaks, you can predict fairly well when another will. It's a little like knowing the time in London if you know the time in New York. But when your normal routine changes, your circadian rhythms may be thrown out of phase. Such internal desynchronization often occurs when people take airplane flights across several time zones. Sleep and wake patterns usually adjust quickly, but temperature and hormone cycles can take several days to return to normal. The resulting jet lag affects energy level, mental skills, and motor coordination (Sack, 2010).
Internal desynchronization also occurs when workers must adjust to a new shift. Efficiency drops, the person feels tired and irritable, accidents become more likely, and sleep disturbances and digestive disorders may occur. For police officers, emergency-room personnel, airline pilots, truck drivers, and operators of nuclear power plants, the consequences can be a matter of life and death. Night work itself is not necessarily a problem: With a schedule that always stays the same, even on weekends, people often adapt. However, many swing and night-shift assignments are made on a rotating basis, so a worker's circadian rhythms never have a chance to resynchronize.
Some scientists hope eventually to help rotating-shift workers and travelers crossing time zones adjust more quickly by using melatonin, drugs, or other techniques to “reset the clock” (van de Werken et al., 2013), but so far these techniques do not seem ready for prime time. Giving shift workers melatonin sometimes helps and sometimes does not; stimulant drugs can improve attention but don't eliminate physical fatigue; and although short naps on the job increase alertness, many employers do not like the idea of paying people to sleep (Kolla & Auger, 2011). When a pilot in Nevada was unable to contact a napping air traffic controller at 2:00 a.m., scientists butted heads with government officials about who was to blame. “There should be sanctioned on-shift napping. That's the way to handle night-shift work,” said one neuroscientist. But the Federal Aviation Administration still bans the practice, while calling for more data.
One reason a simple cure for desynchronization has so far eluded scientists may be that circadian rhythms can be affected by illness, stress, exercise, drugs, mealtimes, and many other factors. Also, circadian rhythms differ greatly from person to person. There truly are morning people (“larks”) and evening people (“owls”). Scientists call your identity as a lark or owl your “chronotype.” Genetic influences may contribute to chronotypes, although early attempts to find “chronotype genes” have proven difficult to replicate (Chang et al., 2011; Osland et al., 2011). Moreover, your chronotype may change as you age: Adolescents are more likely than children and older adults to be owlish (Biss & Hasher, 2012), which may be why many teenagers have trouble adjusting to school schedules. You may be able to learn about your own personal pulses through careful self-observation, and you may want to try putting that information to use when planning your daily schedule.

For at least 3 days, except when you are sleeping, keep an hourly record of your mental alertness level, using this five-point scale: 1, extremely drowsy or mentally lethargic; 2, somewhat drowsy or mentally lethargic; 3, moderately alert; 4, alert and efficient; and 5, extremely alert and efficient. Does your alertness level appear to follow a circadian rhythm, reaching a high point and a low point once every 24 hours? Or does it follow a shorter rhythm, rising and falling several times during the day? Are your cycles the same on weekends as during the week? Most important, how well does your schedule mesh with your natural fluctuations in alertness?
Moods and Long-Term Rhythms
According to Ecclesiastes, “To every thing there is a season, and a time for every purpose under heaven.” Modern science agrees: Long-term cycles have been observed in everything from the threshold for tooth pain to conception rates. Folklore holds that our moods follow similar rhythms, particularly in response to seasonal changes and, in women, menstrual changes. But do they?
Does the Season Affect Moods? Clinicians report that some people become depressed during particular seasons, typically winter, when periods of daylight are short, a phenomenon that has come to be known as seasonal affective disorder (SAD). This condition is relatively uncommon and is not recognized as an official disorder in the leading diagnostic manual used by clinicians (American Psychiatric Association, 2013). During the winter months, SAD patients report feelings of sadness, lethargy, drowsiness, and a craving for carbohydrates. To counteract the effects of sunless days, physicians and therapists often treat SAD patients with phototherapy, having them sit in front of bright fluorescent lights at specific times of the day, usually early in the morning. In some cases, they have also begun prescribing antidepressants and other drugs.

Bright light therapy is often used in the treatment of seasonal affective disorder (SAD). Thirty minutes in front of a lamp such as this one may produce benefits for some people with this uncommon diagnosis.
Unfortunately, much of the research on the effectiveness of light treatments has been flawed; a review of 173 published studies found that only 20 had a proper design and suitable controls (Golden et al., 2005). But a meta-analysis of the data from those 20 studies did throw some light on the subject, so to speak. When people with SAD were exposed to either a brief period (e.g., 30 minutes) of bright light after waking or to light that slowly became brighter, simulating the dawn, their symptoms were in fact reduced. Light therapy even helped people with mild to moderate non seasonal depression (Pail et al., 2011).
SAD may occur in people whose circadian rhythms are out of sync; in essence, they have a chronic form of jet lag (Lewy et al., 2006). Or they may also have some abnormality in the way they produce or respond to melatonin (Wehr et al., 2001). They may produce too much daytime melatonin in the winter, or their morning levels may not fall as quickly as other people's. However, it is not clear why light therapy also appears to help some people with nonseasonal depression. True cases of SAD may have a biological basis, but if so, the mechanism remains uncertain. Keep in mind, too, that for many people who get the winter blues, the reason could be that they hate cold weather, are physically inactive, do not get outside much, or feel lonely during the winter holidays.
Does the Menstrual Cycle Affect Moods? Controversy has persisted about another long-term rhythm, the female menstrual cycle, which occurs, on average, every 28 days. During the first half of this cycle, an increase in the hormone estrogen causes the lining of the uterus to thicken in preparation for a possible pregnancy. At midcycle, the ovaries release a mature egg, or ovum. Afterward, the ovarian sac that contained the egg begins to produce progesterone, which helps prepare the uterine lining to receive the egg. Then, if conception does not occur, estrogen and progesterone levels fall, the uterine lining sloughs off as the menstrual flow, and the cycle begins again. The interesting question for psychologists is whether these physical changes cause emotional or intellectual changes, as folklore and tradition would have us believe.
Most people nowadays seem to think so. They are often surprised to learn that it was not until the 1970s that a vague cluster of physical and emotional symptoms associated with the days preceding menstruation—including fatigue, headache, irritability, and depression—was packaged together and given a label: premenstrual syndrome (PMS) (Parlee, 1994). Since then, most laypeople, doctors, and psychiatrists have assumed, uncritically, that many women “suffer” from PMS or from its supposedly more extreme and debilitating version, “premenstrual dysphoric disorder” (PMDD). What does the evidence actually show?
Figure 5.1
Mood Changes in Men and Women

Other investigations have confirmed that most women do not have typical PMS symptoms even when they firmly believe that they do (Hardie, 1997; McFarlane & Williams, 1994). For example, women often say they cry more premenstrually than at other times, but they are usually wrong. A study of Dutch women who kept “crying diaries” found no association at all between crying and phase of the menstrual cycle (van Tilburg, Becht, & Vingerhoets, 2003).
The really important question is whether the phase of the menstrual cycle a woman is in affects her ability to work, think, study, do brain surgery, run for office, or run a business. In the laboratory, women tend to be faster on tasks such as reciting words quickly or sorting objects manually before and after ovulation, when their estrogen is high (e.g., Saucier & Kimura, 1998). But phase of the menstrual cycle is unrelated to work efficiency, problem solving, grades, college exam scores, creativity, or any other behavior that matters in real life (Earl-Novell & Jessop, 2005; Golub, 1992; Richardson, 1992). In the workplace, men and women report similar levels of stress, well-being, and ability to do the work required of them—and it doesn't matter whether the women are premenstrual, menstrual, postmenstrual, or nonmenstrual (Hardie, 1997).
In sum, the body provides only the clay for our symptoms and feelings. Learning and culture mold that clay by teaching us which symptoms are important or worrisome, and which are not. Whether we are male or female, the impact of most of the changes associated with our biological rhythms depends on how we interpret and respond to them.