12.1
Motivation and the Hungry Animal
Before we begin examining specific motives, it's important to understand what “motivation” means to psychologists in the first place.
Defining Motivation
Describing someone as “motivated” conjures up many possible definitions. Synonyms like striving, craving, goal-oriented, or focused come to mind, but those terms beg for definition as well. A scurrying cockroach appears motivated not to be eaten by a bird, but would you call the roach's behavior “craving”? A general definition of motivation seems necessary, and for most psychologists, it refers to a process within a person or animal that causes that organism to move toward a goal or away from an unpleasant situation.
There are two main sources of motivation. Intrinsic motivation refers to the desire to do something for its own sake and the pleasure it brings. For example, a runner may be motivated to exercise simply because it makes her feel good and energized. A young child may be motivated to read purely because reading is a pleasurable activity. Extrinsic motivation refers to the desire to do something for external rewards, such as money, good grades, or other external enticement. A runner whose motive is to run farther than her next-door neighbor or to win a slew of medals is focused on something different than the intrinsic value of exercise. Similarly, a child who reads only to rack up Good Reader points or get a certificate from the local library may find little pleasure in the world of books. As we see throughout this chapter, whether your motives are intrinsic or extrinsic affects how readily you meet your goals, and how satisfied meeting them can make you feel. Before discussing that, however, let's examine a very basic motive that needs to be met in order to survive: eating.
What Motivates You?

The Biology of Weight
If you've ever been extremely hungry you know how powerful a motive food can be. You become focused only on satisfying your hunger, and accept the first edible morsels you can find rather than puzzling through which delicacy you really crave. But assuming you don't wait to arrive at the brink of starvation before you eat, on a day-to-day level, how much do genes, psychological processes, and the environment affect our motivation to eat, or shape what we choose to eat?
At one time, most psychologists thought that being overweight was a sign of emotional disturbance. If you were fat, it was because you hated your mother, feared intimacy, or were trying to fill an emotional hole in your psyche by loading up on rich desserts. The evidence for such psychological theories of overweight, however, came mainly from self-reports and from flawed studies that lacked control groups or objective measures of how much people were actually eating. When researchers performed controlled studies, they learned that fat people, on average, are no more and no less emotionally disturbed than average-weight people. Even more surprising, researchers found that heaviness is not always caused by overeating (Munsch & Jansen, 2014; Stunkard et al., 2004). Many heavy people do eat large quantities of food, but so do some thin people. In one early experiment, in which volunteers gorged themselves for months, it was as hard for slender people to gain weight as it was for most heavy people to lose weight. After the study was over, the slender people lost weight as fast as dieters gained it back (Sims, 1974). The video Food Cravings and Preferences offers some explanations for why it is easier to gain weight than to lose it.
Watch
Food Cravings and Preferences
Genetic Influences on Weight and Body Shape The explanation that emerged from such findings was that a biological mechanism keeps your body weight at a genetically influenced set point, the weight you stay at—plus or minus 10 percent—when you are not trying to gain or lose (Lissner et al., 1991). Set-point theory generated much research on how the body regulates appetite, eating, and weight gain and loss. Everyone has a genetically programmed basal metabolism rate, the rate at which the body burns calories for energy, and a fixed number of fat cells, which store fat for energy and can change in size. Obese people have about twice the number of fat cells as normal-weight adults do, and their fat cells are bigger (Kopelman, Caterson, & Dietz, 2009). When people lose weight, they don't lose the fat cells; the cells just get thinner, and easily plump up again.

Body weight and shape are strongly affected by genetic factors. Set-point theory helps explain why the Pimas of the American Southwest gain weight easily but lose it slowly, whereas some people from other backgrounds can eat a lot of food yet remain slender.
A complex interaction of metabolism, fat cells, and hormones keeps people at the weight their bodies are designed to be, much in the way that a thermostat keeps a house at a constant temperature. When a heavy person diets, the body's metabolism slows down to conserve energy and fat reserves (Harrington et al., 2013). When a thin person overeats, metabolism speeds up, burning energy. In one study, in which 16 slender volunteers ate 1,000 extra calories every day for 8 weeks, their metabolisms sped up to burn the excess calories. They were like hummingbirds, in constant movement: fidgeting, pacing, changing positions frequently while seated (Levine, Eberhardt, & Jensen, 1999).
What sets the set point? Genes, to start with. Pairs of adult identical twins who grow up in different families are just as similar in body weight and shape as twins raised together. And when identical twins gain weight, they gain it in the same place: Some pairs store extra pounds around their waists, others on their hips and thighs (Comuzzie & Allison, 1998; Horn et al., 2015). Genes also influence how much brown fat a person has in addition to the usual white fat. Brown fat is an energy-burning type of fat that seems important in regulating body weight and blood sugar. It is lacking in obese people, which may be one reason that fat people can't burn all the calories they consume (Cypess et al., 2009). However, production of brown fat is also triggered by cold and exercise, which, in mice at least, turns ordinary white fat brown (Ouellet et al., 2012). Brown fat cells are fascinating; when they run out of their own sources of energy, they suck fat out of the rest of the body to keep their proprietor warm. Sorry, you can't (yet!) order a brown-fat supplement online.
Gene Mutations and Leptin When a mutation occurs in the genes that regulate normal eating and weight control, the result may be obesity. One gene, called obese, or ob for short, causes fat cells to secrete a protein, which researchers have named leptin (from the Greek leptos, meaning “slender”). Leptin travels through the blood to the brain's hypothalamus, which is involved in the regulation of appetite. When leptin levels are normal, people eat just enough to maintain their weight. When a mutation of the ob gene causes leptin levels to be too low, however, the hypothalamus thinks the body lacks fat reserves and signals the individual to overeat. Injecting leptin into leptin-deficient mice reduces the animals' appetites, speeds up their metabolisms, and makes them more active; as a result, the animals shed weight. Alas, for most obese people, and for people who are merely overweight, taking leptin does not produce much weight loss (Comuzzie & Allison, 1998).
Studies of mice suggest that leptin plays its most crucial role early in life, by altering the brain chemistry that influences how much an animal or person later eats. More specifically, leptin helps regulate body weight by strengthening neural circuits in the hypothalamus that reduce appetite and by weakening circuits that stimulate it (Elmquist & Flier, 2004). During a critical period in infancy, leptin influences the formation of those neural connections, and the set point is, well, set (Bouret, Draper, & Simerly, 2004). Some researchers speculate that because of this early neural plasticity, overfeeding infants while the hypothalamus is developing may later produce childhood obesity.

Both of these mice have a mutation in the ob gene, which usually makes mice chubby, like the one on the right. But when leptin is injected daily, the mice eat less and burn more calories, becoming slim, like his friendly pal. Unfortunately, leptin injections have not had the same results in most human beings.
Other Factors in Obesity Numerous other genes are linked to being overweight or obese (Farooqi & O'Rahilly, 2004; Frayling et al., 2007; Herbert et al., 2006; Stice et al., 2008). One gene modulates production of a protein that apparently converts excess calories into heat rather than fat. You have receptors in your nose and mouth that keep urging you to eat more (“The food is right there! It's good! Eat!”), receptors in your gut telling you to quit (“You've had enough already!”), and leptin and other chemicals telling you that you have stored enough fat or not enough. The hormone ghrelin makes you hungry and eager to eat more, and leptin turns off your appetite after a meal, making you eat less. This complex set-point system seems to explain why dieters who lose weight so rarely keep it off. Even a year after their weight loss, the bodies of dieters are still leptin deficient, sending out hormonal signals to eat more and restore the lost pounds (Kissileff et al., 2012).
As if all this weren't enough, your brain will get high on sugary foods even if your tongue can't taste them or enjoy their texture. Sweets increase pleasure-inducing dopamine levels in the brain, making you crave more rich food (de Araujo et al., 2008). (Forget about trying to fool your brain with artificial sweeteners; they just make you want the real thing.) Some obese individuals may have underactive reward circuitry, which leads them to overeat to boost their dopamine levels (Stice et al., 2008). When heavy people joke (or lament) that they are “addicted” to rich food, they may be right.
The complexity of the mechanisms governing appetite and weight explains why appetite-suppressing drugs inevitably fail in the long run: They target only one of the many factors that conspire to keep you the weight you are.
But efforts to sell weight-loss products, surgeries, and programs thrive because 69 percent of adults and at least 35 percent of children and teenagers in the United States are now overweight or obese, according to recent figures from the Centers for Disease Control and Prevention. Increases in obesity rates have occurred in both sexes, all social classes, and all age groups, and in many other countries (Popkin, 2009), including Mexico, Egypt, North Africa, Canada, Great Britain, Japan, and Australia, and even coastal China and Southeast Asia. Many health researchers are worried about this trend because obesity is considered a leading risk factor in type 2 diabetes, high blood pressure, heart disease, stroke, and other disorders. (Some experts, however, think that these health concerns have been exaggerated because many overweight people are otherwise fit and in good cardiovascular health, and many thin people are not [Wildman et al., 2008].) But a puzzle remains: If genes and all the chemical factors and fat cells they regulate are so strongly implicated in weight, why are so many people, all over the world, getting fatter?
Implicit Associations Test

Environmental Influences on Weight
The leading culprits causing the worldwide rise in weight have to do with five big changes in the environment and several less obvious ones:
The increased abundance of fast food and processed foods that are inexpensive, readily available, and high in sugar, starch, and carbohydrates (Monteiro et al., 2013). Human beings are genetically predisposed to gain weight when rich food is abundant because, in our species' evolutionary past, starvation was all too often a real possibility. Therefore, a tendency to store calories in the form of fat provided a definite survival advantage. Unfortunately, evolution did not produce a comparable mechanism to prevent people who do not have hummingbird metabolisms from gaining weight when food is easily available, tasty, rich, varied, and cheap. That, of course, is precisely the situation today, surrounded as we are by 3/4-pound burgers, fries, chips, tacos, candy bars, pizza, and soda.
One research team followed thousands of ninth-grade schoolchildren, before and after a new fast-food restaurant opened near their schools. Those whose schools were within a block of a burger or pizza outlet were more likely to become obese in the next year than students whose schools were a quarter of a mile or more away (Currie et al., 2009). Proximity to fast food seems to be a major cause of the “freshman 15” as well. In a study at two very different universities, one in the Midwest and the other on the East Coast, more than 70 percent of all first-year students gained significant amounts of weight (Lloyd-Richardson et al., 2009).
The widespread consumption of high-sugar, high-calorie soft drinks. Throughout most of human history, the proportion of calories consumed in beverages (milk, wine, fruit juice, and the like) was low, and thus the human body did not evolve a mechanism that would compensate for fluid intake by lowering food intake. Then, 50 years ago, soft drinks, which are loaded with sugar and calories, began spreading across the globe. Putting sweeteners into drinks has led to a weight gain of up to 14 pounds per person in those who drink two to three sodas a day (Powell & Popkin, 2013).
The sharp decline in exercise and other expenditures of energy because of remote controls, a preference for sedentary activities such as watching television and playing video games, and the speed and convenience of driving rather than walking or biking.
The increased portion sizes of food and drinks. Servings of food and drinks have become supersized, double or triple what they were only one generation ago. Even babies and toddlers are being fed as much as 30 percent more calories than they need (Fox et al., 2004). In France, people eat rich food but much less of it than Americans do. Their notion of what a proper portion is—for yogurt, soda, a salad, a sandwich, anything—is much smaller than in the United States (Rozin et al., 2003).
The abundance of highly varied foods. When diets are predictable, people habituate to what they are eating and eat less of it. That is why all diets that restrict people to eating only a few kinds of foods (only watermelon, only protein, only whatever) are successful at first. As soon as food becomes more varied, however, people eat more and gain more weight (Remick, Polivy, & Pliner, 2009). In fact, people will even eat more M&Ms when they are available in a bowl containing 10 colors than when the same number of candies are in a bowl containing only seven colors (Wansink, 2006).
In addition to these obvious causes, researchers have identified other suspects in the mystery of increasing obesity. One is sleeplessness. Sleep plays an important role in regulating weight, and many infants, children, and adults are simply not getting enough of it (Bell & Zimmerman, 2010). Another is a woman's excessive weight gain during pregnancy—something at one time recommended but that is now known to produce infants of higher-than-normal birth weight, who then have a greater risk of becoming obese adults because of the metabolic changes we mentioned earlier (Ludwig & Currie, 2010). A third possibility is central heating and air conditioning, which keep people from shivering and burning brown fat in winter and sweltering (and therefore eating less) in summer. And yet another candidate is exposure to cold viruses: Children exposed to adenovirus-36 are more likely to become obese than children who are not infected, and this link has been found in adults in Korea and Italy as well as in the United States (Gabbert et al., 2010). The virus was first isolated in the late 1970s, when obesity rates began to climb. Obesity itself is not contagious—the virus is long gone after a person has gained the weight—but someone could catch the virus from a thin person who harbors it.
Ultimately, the obesity puzzle requires us to apply the critical-thinking guidelines “be willing to wonder,” “tolerate uncertainty,” and “consider other explanations.” When David Allison, an obesity researcher, observed significant weight gain among a colony of research marmosets, with no obvious causes due to changes in exercise or amount of food, his curiosity was aroused. He and his colleagues examined 24 samples from eight species, domestic and wild, in different environments, totaling some 20,000 animals. Weight increases over a decade varied from 3 percent (in dogs) to 21 percent (in wild rats), but all species showed an average weight gain (Klimentidis et al., 2011). These animals aren't watching TV or drinking gallons of soda! Perhaps, however, they are eating more human junk food, provided by their human owners or found in the trash. Or perhaps some as-yet-undiscovered environmental factors that animals and humans share will one day provide the answer.
What's Controlling What You Eat?

The Body as Battleground: Eating Disorders
Some people lose the battle between the body they have and the body they want, developing serious eating disorders that reflect an irrational terror of being fat. In bulimia nervosa, the person binges (eats vast quantities of rich food) and then purges by inducing vomiting or abusing laxatives. In anorexia nervosa, the person eats hardly anything and therefore becomes dangerously thin; people with anorexia typically have severely distorted body images, thinking they are fat even when they are emaciated. Anorexia has the highest mortality rate of all mental disorders; many of its sufferers die of heart or kidney failure or complications brought on by weakened bones. To learn more about these disorders, watch the video Eating Disorders.
Watch
Eating Disorders
Bulimia and anorexia are the most well-known eating disorders, and occur most often among young white women. But more than 40 percent of all cases of eating disorders occur among men, older adults, ethnic minority groups, young children, and athletes, and do not fit the diagnostic criteria for bulimia or anorexia (Thomas, Vartanian, & Brownell, 2009). People with binge-eating disorder binge without purging; others chew whatever food they want but spit it out without swallowing; others are normal weight but take no joy in eating because they worry obsessively about gaining a pound; some develop phobias about eating certain kinds of food. All of these disorders involve an unhealthy attitude toward food, weight, and the body.
Genes play a role in the development of some eating disorders, particularly anorexia nervosa, which has been found across cultures and throughout history (Striegel-Moore & Bulik, 2007). But most disorders are generated by psychological factors, including depression and anxiety, low self-esteem, perfectionism, and a distorted body image (Hilbert et al., 2014; Presnell, Bearman, & Stice, 2004; Sherry & Hall, 2009). Cultural factors can also generate dissatisfaction with one's body. Bulimia is rare to nonexistent in non-Western cultures and has only become a significant problem in Western cultures with the rise of the thin ideal for women (Keel & Klump, 2003). A meta-analysis of experimental and correlational studies found that women's exposure to the media ideal of impossibly thin women fosters the belief that “thin is beautiful” and increases the risk of disordered eating (Grabe, Ward, & Hyde, 2008; Slevec & Tiggemann, 2011). American culture is also rife with body snarking, the relentlessly critical and snide appraisals of other people's bodies that get posted on blogs, YouTube, Facebook, and Twitter, and are constant topics for entertainment magazines and talk shows (Boepple & Thompson, 2015).
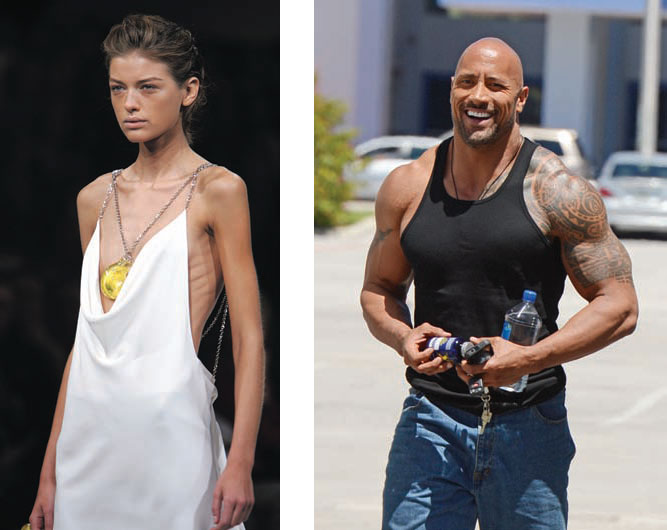
Some argue that the increased prevalence of anorexia and other eating disorders is a product of girls and women seeing ultra-thin fashion models on the pages of magazines. Meanwhile, eating disorders and body image distortions among boys and men are increasing too, as the “ideal” male evolves into a more bulky, muscular shape. What do you think?
So perhaps it is no wonder that in the United States, women's dissatisfaction with their bodies now crosses all ethnic lines; the levels among Asian American, African American, Hispanic, and Anglo women are virtually the same (Grabe & Hyde, 2006). Eating disorders and body image distortions among boys and men are increasing too, though they take different forms. Just as anorexic women see their gaunt bodies as being too fat, some men have the delusion that their muscular bodies are too puny, so they abuse steroids and exercise or pump iron compulsively (Thompson & Cafri, 2007). In contrast, Chinese men in Taiwan and pastoral nomads of northern Kenya do not think the heavily muscled male body is especially desirable or attractive, and their cultures do not promote media images of muscular males. Men in these cultures have fewer body image disorders than American men do and virtually no interest in muscle-building drugs (Campbell, Pope, & Filiault, 2005; Yang, Gray, & Pope, 2005).
In sum, within a given environment, genetic predispositions for a certain body weight and metabolism interact with psychological needs, cultural norms, and individual habits to shape, in this case quite literally, who we are.